The myth of healthy obesity — what tests hide.

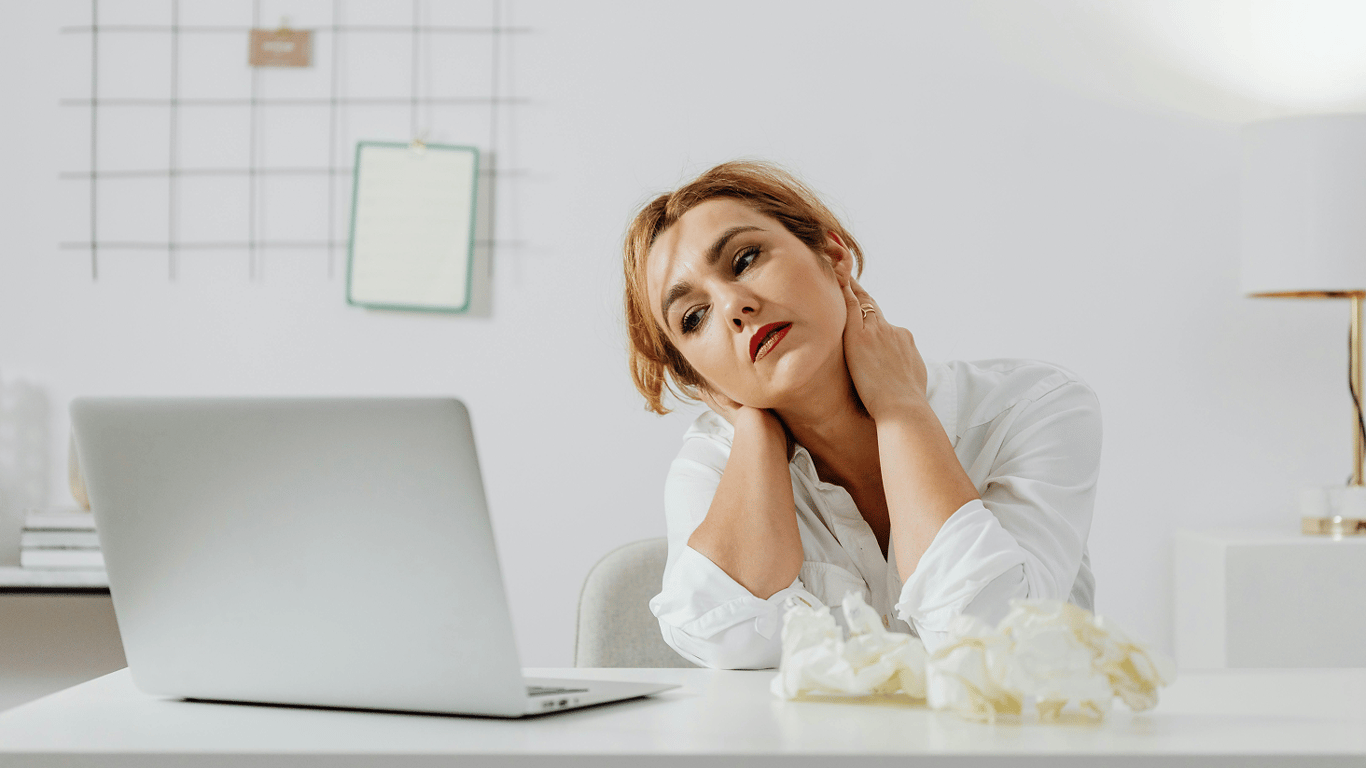
A 38-year-old woman, with no chronic diagnoses, has a BMI of 32. Her blood pressure is normal, and her tests show no critiques. She regularly exercises, monitors her glucose and cholesterol levels. But during her visit to the cardiologist, she hears the same old question: 'Are you working on your weight?'It sounds unfair, doesn’t it? All her indicators are good. So why is her heart still at risk? Is obesity really an independent threat factor, even if the metabolic profile is normal? And what do recent studies say about so-called 'healthy obesity'?
Obesity and the heart — what is their dependency?
Being overweight is not just about aesthetics. For the heart, it literally means physical strain. The cardiovascular system works under more complex conditions due to obesity: the volume of blood that needs to be pumped increases, as does the pressure on the vessels. This raises the risk of hypertension, ischemic heart disease, and heart failure.The American Heart Association published a large review of studies in 2021: even with normal blood pressure, cholesterol, and glucose levels, obesity itself is associated with an increased risk of cardiovascular events (
Polednak, 2021). This applies to both women and men.
'Healthy obesity' — a myth?
The term 'metabolically healthy obesity' (MHO) indeed exists in literature. It refers to people with a raised BMI (over 30), but without accompanying metabolic disorders. However, reviews (
Bluher, 2021, Nature Reviews Endocrinology) indicate that this condition is often temporary — it often progresses into 'unhealthy obesity' with all its consequences over the years.Another study (
Caleyachetty et al., 2017, European Heart Journal) confirms: people with MHO have a higher risk of cardiovascular diseases than those with normal weight, even if other indicators are normal. This means that weight is an independent risk factor.
Why BMI doesn’t always show the full picture
Body mass index is a convenient but crude tool. It does not account for the ratio of muscle to fat, nor the distribution of fat tissue. Most importantly, it is visceral fat (around internal organs) that is the main risk factor. It influences metabolism, inflammation levels in the body, and insulin resistance.Thus, even with a normal BMI, a person can have excess visceral fat — and conversely, have a high BMI but a healthy metabolic profile (even if not for long).
What to do about this — a care strategy
The main thing is not stigmatization, but awareness. A patient with a BMI of 32, who goes to the gym and gets tested — this is not a 'bad patient', but a person who is already in the process of change. The doctor’s task is to support and explain that fat tissue is not inert, it is hormonally active and affects blood vessels, pressure, and heart function.We cannot change the body in a day, but we can:
- track waist size (a more accurate risk marker than BMI);
- maintain regular physical activity;
- monitor nutrition, without extreme diets;
- get tested annually: lipid profile, glucose, blood pressure;
- work with a doctor — without judgment, but with responsibility.
Obesity is not a sentence, but a risk factor. Even in its 'metabolically healthy' variant — it is not the norm, but a call to action. The heart does not see the number on the scales. But it certainly feels how much every extra kilogram weighs.
The message addresses the relationship between obesity and heart condition. The data from studies show that regardless of other medical indicators, obesity can be a risk factor for cardiovascular diseases. Therefore, it is essential to maintain awareness and conduct regular monitoring of one's health to prevent possible complications, even in the case of 'healthy' obesity.Read also
- How to Survive an Abnormal Heatwave - Medical Advice
- Even after vacation — why most people are constantly tired
- How to Get Rid of Gray Hair at Any Age - Simple Solutions
- The Genes of Youth - How Habits Affect Biological Age
- OCHMATDYT Repair - Director General Reveals When Works Will Be Completed
- HIV status - can such citizens be mobilized